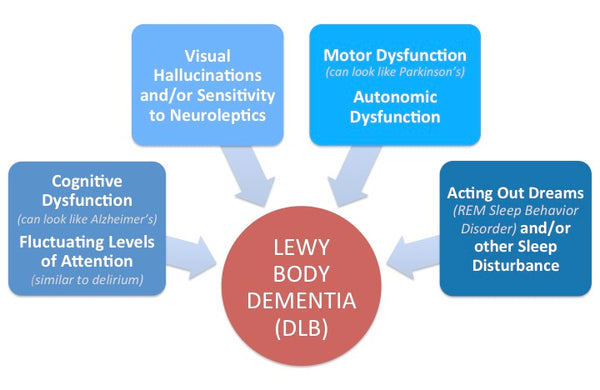
LBD (Lewy Body Dementia), or Dementia with Lewy Bodies (DLB), is a neurodegenerative disease that has characteristics similar to that of both Alzheimer’s and Parkinson’s diseases. It is one of the four common types of dementia known and is associated with protein deposits in the brain that cause disruptions to the normal functioning of the brain. Diagnosing the disease is extremely tough as its symptoms can resemble that of other brain diseases.
The Lewy Body Disease Family

Lewy Body Dementia is a member of the Lewy Body Disease Family which includes (1) Lewy Body Dementia (LBD) often times called Dementia with Lewy Bodies (DLB), (2) Parkinson's Disease (PD) and (3) Parkinson's Disease with Dementia (PDD). Although we talk a little about PD and PDD throughout the guide below but we focus primarily on LBD.
Scroll down for all of the juicy details of Lewy Body Dementia! Make sure to use the Quick Links and "Return to Section List" Links throughout the article to move quickly through the info!
TOPICS COVERED - QUICK LINKS:
- WHAT IS LEWY BODY DEMENTIA?
- WHO DOES LBD AFFECT?
- WHAT CAUSES LBD?
- SYMPTOMS
- DIAGNOSING LBD CORRECTLY
- LBD VS. PARKINSON’S
- TREATMENT
- CHALLENGES OF CARING FOR AN LBD PATIENT
- CARE ARRANGEMENTS FOR LBD PATIENTS
- RESEARCH AND CLINICAL TRIALS
- RESOURCES, SUPPORT AND OTHER WEBSITES
- IN THE NEWS
WHAT IS LEWY BODY DEMENTIA?
One of the most common causes of dementia after Alzheimer’s disease and vascular dementia, LBD occurs due to abnormal microscopic deposits of a protein known as alpha-synuclein in the brain. Discovered in the early 1900s by Freiderich H. Lewy, these proteins are better known as Lewy bodies. The build-up of these Lewy bodies causes the brain to deteriorate due to the disruption of normal brain functioning.
In normal conditions, the alpha-synuclein proteins are actually quite abundant in the brain. The problem of LBD arises when the proteins mutate and form little clusters within neurons, which leads to cellular death. The location of the protein deposits define the types of symptoms that a person exhibits. It can be either that of Parkinson’s, which mainly affects the motor system, or that of Alzheimer’s, which mainly affect cognition and memory.
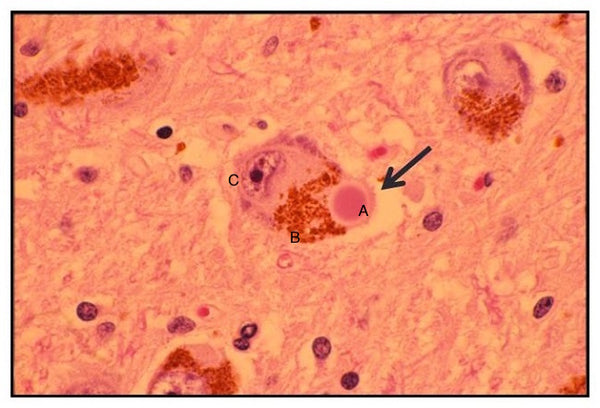
Lewy Body Pathology: H&E Stain
(A) The large pink Circle is a Lewy Body within a Brain Cell. (B) The brown section to the left of the Lewy Body is normal brain pigmentation. (C) The nucleus, the cell's control center is to the far left of the cell.
(Source: US Department of Health & Services: Advisory Council on Alzheimer's Research, Care and Services)
More Information
- In the News: Lewy Body Dementia (LBD)
WHO DOES LBD AFFECT?
Lewy Body Dementia accounts for roughly 4% of all recorded dementia. However, experts believe that, due to its symptoms overlapping with other brain disorders, it is severely underdiagnosed and could possible account for more than 10% of all dementia cases. It is estimated that 1.4 Million Americans have LBD, PDD, or LBV-AD. In terms of gender, LBD tends to affect males and females equally.
Age on the other hand, plays an important role. Most cases of LBD are found in individuals in their mid-60s and beyond. The onset of the disease prior to that is quite rare. Other risk factors include, medical, lifestyle, and environmental are known to increase a person’s chances of developing LBD. Once in a while, the onset of LBD can be genetically linked, but these are special occurrences and require further research to support.
More Information
- In the News: Prevention
WHAT CAUSES LBD?
Unfortunately, the exact cause of Lewy Body Dementia remains unknown to date and is still an area that has much to be studied. Researchers believe that there might be a hereditary link to the disease, but have yet to find strong support for it.
What is known about the disease is that it occurs when a mutated form of the alpha-synuclein protein (Lewy bodies) start to accumulate in the brain. These clusters of protein deposits seem to cause a decrease in the neurons’ communication capabilities. Two possible areas of the brain that it usually affects are the brain stem or cerebral cortex, which results in a deteriorated motor system or cognition and memory respectively.
Brain Scans: Progression of Lewy Body Dementia

(Source: Blog - Going Gentle Into that Good Night)
More Information
- In the News: Causes
SYMPTOMS
Unlike Alzheimer’s, the symptoms of LBD cannot be classified into concrete stages as it manifests differently in each person. One person might show one combination of symptoms while another person might display a different combination of symptoms. They may even fluctuate between normal and abnormal conditions from day to day, hour to hour, or even moment to moment. Overall, the symptoms of LBD can be classified into initial, core, suggestive, and supportive features. However, the central feature is the same as other dementias: progressive dementia, where memory, attention, and executive function deteriorate over time.
The Beginning
Core Features
Suggestive Features
Supportive Features
More Information
- In the News: Symptoms
DIAGNOSING LBD CORRECTLY
Diagnosing LBD in patients correctly is very difficult. The biggest challenge to this is the overlapping symptoms in a patient that can resemble other neurodegenerative disorders or other completely different illnesses altogether. The only way to be very sure of a diagnosis is in post-mortem situations—when the brain tissue can be examined under a microscope and Lewy Bodies can be found.
Nevertheless, it is possible to increase the chances of correctly diagnosing LBD by ruling out other causes of the person’s symptoms and following the timeline of its occurrences closely. This could be done through blood tests, a variety of brain scans, memory tests, physical tests, psychological evaluation, and more.
Doctors can diagnose a person’s symptoms as either Probably LBD or Possible LBD. Each of has its own set of criteria. In order for it to be considered Probably LBD, the patient must have dementia and at least two of the core features listed in the symptoms. Another way for it to be considered as Probably LBD is if the patient has one core feature and at least one suggestive feature in addition to dementia. For the diagnosis to be Possible LBD, the patient must have dementia and one core feature or at least one suggestive feature.

(Source: Lewy Body Dementia Association)
More Information
- Lewy Body Dementia Association: Diagnosis
- In the News: Detection and Diagnosis
LBD VS. PARKINSON’S
LBD is typically listed as a type of dementia. But what is often not known is that it is actually a spectrum of disorders involving disturbances of movement, cognition, behavior, sleep, autonomic functions. Experts distinguish two key forms within this spectrum: Dementia with Lewy Body and Parkinson’s disease Dementia. Depending on where the Lewy bodies are present in the brain, the symptoms and therefore the diagnosis will be different.

(Source: Lewy Body Dementia Association)
When the Lewy bodies are found in the outer layers of the brain (cerebral cortex), it is mostly linked to problems with mental abilities, which are characteristic of Dementia with Lewy Body. Acetylcholine is depleted in this case, causing disruption of perception, thinking, and behavior. For Parkinson’s on the other hand, the Lewy bodies accumulate at the base of the brain where a person’s motor movements are controlled. Here, the dopamine neurotransmitters are depleted, causing the symptoms to appear.
Another distinction between the two is the timeline of diagnosis. Dementia with Lewy Body is diagnosed when dementia has already been present within one year of the onset of motor symptoms. Parkinson’s dementia on the other hand is diagnosed if the onset of dementia occurs at least a year after the onset of motor symptoms. The one year cut-off time is the generally accepted period by most clinicians.
Brain Scans: Comparing LBD vs. AD vs. PD

(Source: Neurology.net - Imaging Amyloid Disposition in Lewy Body Dementia's)
Back to the Section ListTREATMENT
As is the case with most forms of dementia, there is currently no cure for LBD. However, most of the symptoms presented are treatable and can help to slow down the progression of the disease.
Medication
- Cognitive Issues: Confusion, Behavioral Issues, Alertness
- Movement Disorders: Help to treat Parkinson-like symptoms.
- Psychological Symptoms: Antidepressants, Antipsychotics
Treatments
- Psychological and Behavioral Therapy
- Physical Therapy
- Occupational Therapy
- Speech Therapy and Swallowing Therapy
More Information
Back to the Section ListCHALLENGES OF CARING FOR AN LBD PATIENT
In general, caring for someone with dementia is very challenging and LBD cases are no different. The caregiver will face challenges with the patient’s inability to solve problems, change of daily routine, and lack of stamina. However, there are a few things that a caregiver can implement to ease the difficulty of caring for an LBD patient. They are:
Learn, Plan and Seek Professional Help:- Learn and Educate: Read up on Lewy Body and seek to find a support system for your loved one diagnosed and yourself. There are others out there who have been through what you are experiencing that are ready to lend a helping hand. Visit our Support and Resources section to start finding a strong community for you to lean on.
- Find Appropriate Medical Assistance: An estimated 80% of dementia patients seek all of their medical attention from their primary care physicians. While the primary care physicians might know the patient intimately from years of going to their practice, dementia patients can require extensive medical assistance especially as behavioral and physical changes occur. Seeking a medical group that specializes in dementia care can generate great relief as they will be equipped with disease specific information and resources for the diagnosed and their families.
- Plan appropriate care arrangements, and address legal, financial and medical long-term care arrangements. Having difficult conversations with your loved one about what to do as situations arise throughout the disease is extremely important. This eases the guilt burden when a loved one is no longer able to advocate for their own wishes. Perhaps the diagnosed has left behind a Will where they address how they wish to manage care and difficult medical situations. As the person's ability to manage their own affairs deteriorates, typically, a spouse, or close relative (children, siblings) will be assigned the Power of Attorney.
- Get adaptive aids to help the person stay active and independent as long as possible (e.g. special eating utensils, walkers, etc.). For tips on how to keep a loved one safe and how to adapt the home for Lewy Body Dementia, check out our Top 11 Safety Concerns for Dementia with Solutions post.
- Creating a routine, especially around meal and bed times is critical to keeping the individual stable and healthy.
- Breaking tasks into smaller steps and focus on success.
- Walking and exercising to improve the person’s mental health as well as decrease muscle stiffness.
- Keeping hydrated in order to avoid low blood pressures which could lead to unexpected falls or injuries.
- Using strategies that help the person get a rhythm for movement (count, clap, hum).
- If person has swallowing problems, vary texture and temperature of food between bites to aid reflexes (e.g. hot or cold, soft of chewy..).
- Validating the person's beliefs and hallucinations, working around them (e.g. escort "visitors" our of the house if they are causing the person to be upset, etc.)
- Being aware that memory isn't affected or is only mildly affected.
- Seek Support for yourself. Caring for someone with dementia is exhausting and you have to remember that you must be ok first in order to care for someone else.
CARE ARRANGEMENTS FOR LBD PATIENTS
When a person is diagnosed with LBD, it is natural that their loved ones would prefer to become the primary caregiver. However, you should take into consideration the LBD progression in the patient and the primary caregiver’s ability and availability to care for them as it can get very challenging. In the initial stage when a person’s symptoms tend to fluctuate, the primary caregivers should be patient when interacting with them. You should always be aware to not embarrass them. Seeking professional psychiatric help can help to mentally cope with their diagnosis.
Once the symptoms are more prevalent, arrangements can be made for the primary caregiver to seek part-time help or in-home care, where trained professionals such as in-home care providers, companionship and personal carers, and medical carers, who help to follow the patient’s routines and keep them pursuing mental and physical activities that can help to stave off worsening symptoms.
However, during the late stages, when the person with LBD is completely dependent on their primary caregiver, the best option most likely would be full-time professional care. While the primary caregiver can still opt to take care of the patient themselves, it can be tiring and mentally draining. Therefore, there is nothing wrong in seeking professional help to ease the burden. External care arrangements in this situation range from full time in-home to residential care.
Back to the Section ListRESEARCH AND CLINICAL TRIALS
Compared to Alzheimer’s, LBD is still a relatively unknown type of dementia. And because of that, there are a lot of ongoing research and clinical trials going on every day. For example, there are:
- Treatment trials where new and existing drugs are tested to study it has a positive effect on the symptoms of LBD.
- Genetics studies where scientists try to figure out whether LBD is a genetically passed down disease.
- Diagnostic studies where scientists and researchers look for better and improved alternative ways of diagnosing the onset of LBD.
- Prevention trials where researchers investigate ways of preventing the onset of LBD itself.
For more information on research currently being conducted on Lewy Body Dementia, the following are great resources and tools that can help shine light on progress being made.
For a list of clinical trials check out these awesome resources:
- ClinicalTrials.gov: Provides regularly updated information about federally and privately supported clinical research in human volunteers. ClinicalTrials.gov gives you information about a trial's purpose, who may participate, locations and phone numbers for more details.
- NIH Clinical Research Trials and You: Is an online resource to help people learn more about clinical trials, why they matter and how to participate. Provides information on the basics of clinical trial participation, first hand experiences from actual clinical trial volunteers, explanations from researchers, and links on how to search for a trial or enroll in a research matching program.
- Fox Trial Finder: Is a web-based clinical trial matching tool to connect those with and without Parkinson's disease to Parkinson's clinical research participation opportunities. Also provides the opportunity for volunteers to connect directly with trial coordinators through a secure messaging interface on the site.
- Alzheimer's Association: Lists selected trials in treatment and prevention of Alzheimer's disease from ClinicalTrials.gov. Trials included here are recruiting participants at more than one U.S. location.
- Center Watch: Clinical research, including listings of more than 41,000 active industry and government-sponsored clinical trials, as well as new drug therapies in research and those recently approved by the FDA.
RESOURCES, SUPPORT AND OTHER WEBSITES
For family members and friends who would like to educate themselves further on the details of Lewy Body Dementia, its symptoms, treatments, and challenges, you should seek the assistance of the national Lewy Body Dementia Association as well as other organizations listed below:
Support Groups
-
Lewy Body Dementia Association: Support Group Listing
-
Online Forums & Chat Rooms:
- Lewy Body Dementia Association Forum: Lewy Body Dementia Association Forum
-
Alzheimer's Association: AlzConnected
- Facebook Groups:
-
Anonymous chat rooms for Free therapy: 7 Cups
IN THE NEWS - LEWY BODY DEMENTIA
Click the following links for News Articles on Lewy Body Dementia (LBD):
Back to the Section List